Colorectal cancer is the second most commonly diagnosed cancer in women, which is why your OB/GYN is likely to be concerned about this disease and include testing or screening options as part of your well-woman’s visit past age 40. Because colorectal cancer is surprisingly common and treatment outcomes improve when it is diagnosed early, it’s important to understand the risk factors, symptoms, and screening options for this disease.
What is Colorectal Cancer?
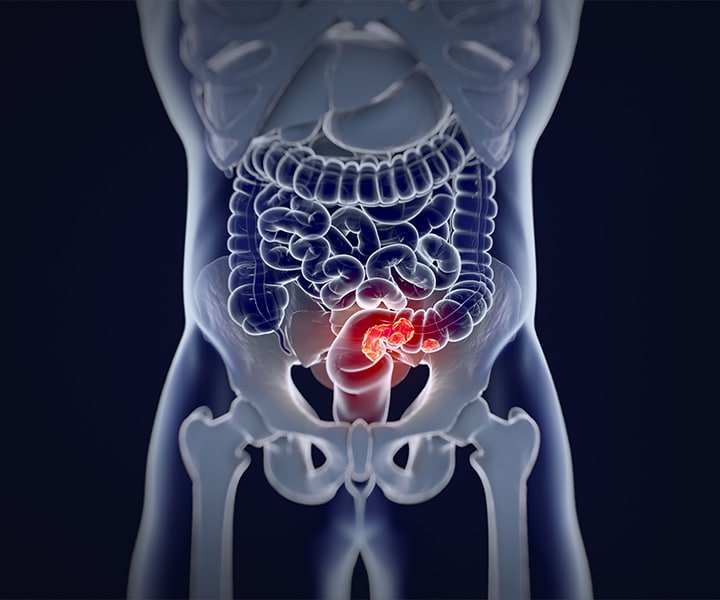
Colon and rectal cancer are cancers that involve the lower digestive tract, including the large intestine (colon) and the rectum. For patients with colorectal cancer, the cells of the large intestine or rectum grow abnormally and out of control. These cancer cells typically begin as polyps.
What are Increased Risk Factors for Colorectal Cancer?
Both genetic and environmental factors can pose increased risk for colorectal cancer. Colorectal cancer is uncommon before age 40, so age is a significant risk factor. Your risk for colorectal cancer increases significantly each decade you age after turning 40.
Family history is also a risk factor for colorectal cancer. You may be at an increased risk if you have an immediate family member (parent, child, or sibling) who was diagnosed with colorectal cancer before age 60. Those with two or more family members who were diagnosed at any age are also considered at a higher risk.
Obesity, a sedentary lifestyle, unhealthy diet, or smoking all increase your risk for colorectal cancer.
If you have an inflammatory bowel disease, including ulcerative colitis or Crohn’s disease, you are also at an increased risk for colorectal cancer. In addition, those who received abdominal radiation as children may be at an increased risk.
Finally, being African American is considered a risk factor for colorectal cancer.
What are the Symptoms of Colorectal Cancer?
Some common symptoms of colorectal cancer include:
- Changes in bowel habits (constipation or diarrhea)
- Rectal bleeding or blood in stool
- Anemia
- Cramping or abdominal pain
- Increased gas pain
- Unintended weight loss
If you notice any of these symptoms, you should schedule an appointment with your doctor, especially if you also have increased risk factors for colorectal cancer.
Can You Test Genetics for Colorectal Cancer?
Several genetic disorders are associated with a high risk for colorectal cancer, so it is possible to have your DNA tested to determine whether you are at an increased risk. Genetic disorders including familial adenomatous polyposis (FAP), MUTYH associated polyposis (MAP), and Lynch syndrome (HNPCC) all present a higher risk for colorectal cancer and can be detected through a blood test. If you are found to have one of these genetic disorders, it is not guaranteed that you will eventually get colorectal cancer. However, your doctor will likely suggest more frequent or earlier screenings.
How Do Doctors Screen for Colorectal Cancer?
Screening or follow-up testing for colorectal cancer is determined by your age, family or genetic history, prior testing findings, and whether you have any colorectal cancer symptoms. Some common screening options for colorectal cancer include:
- Stool testing
- CT colonography
- Colonoscopy
- Capsule colonoscopy
- Flexible sigmoidoscopy
Of the screening options, colonoscopy is the most sensitive. Your doctor will explain which screening option is recommended for you and why.
Schedule an Appointment
To learn more about your screening options and risk for colorectal cancer, schedule an appointment with Carnegie Women’s Health. Call our New York, NY office at (315) 628-7063 or request an appointment online.
Frequently Asked Questions
Is colorectal cancer treatable?
Colorectal cancer is treatable and often curable when localized to the bowel. Surgery is the most common form of treatment and often cures about 50% of patients.
What are the screening options for colorectal cancer?
Some screening test options for colorectal cancer include flexible sigmoidoscopy, colonoscopy, double contrast barium enema, and fecal occult blood tests. Your doctor will recommend your best option after an appointment.
What are the warning signs of uterine cancer?
Abnormal vaginal bleeding and/or discharge is the most common symptom of uterine cancer.
What are the first symptoms of colorectal cancer?
Common symptoms include a persistent change in bowel habits, rectal bleeding, persistent abdominal discomfort, weakness, and fatigue.
What is a polyp?
Polyps are growths that are found in the lining of the colon as a result of out-of-control cell growth.
How common is colorectal cancer?
Colorectal cancer is the third most common type of cancer in the United States.